What Mode Should Be Selected for Defibrillation in Patients with Cardiac Arrest?
1. For patients with cardiac arrest, electrical defibrillation is selected. Clinically, cardiac arrest can be classified into ventricular fibrillation, electromechanical dissociation, asystole, and ventricular fibrillation. Currently, electrical defibrillation is considered the most effective method to terminate ventricular fibrillation, including pulseless ventricular tachycardia.

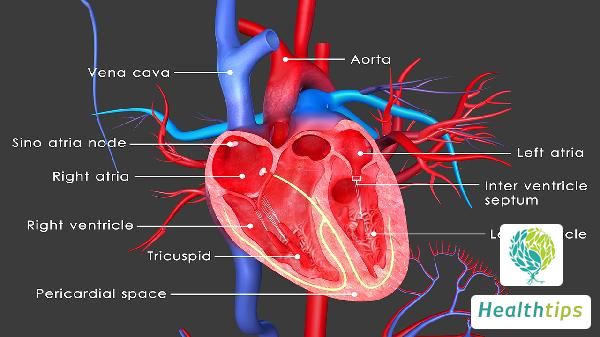
2. Electrical defibrillation is a method that uses a certain amount of electrical current to shock the heart, thereby stopping ventricular fibrillation. Generally, the energy released by the defibrillator is the minimum energy required to terminate ventricular fibrillation. If the chest is open, the electrode pads can be placed directly on the ventricular wall for electrical shocking, which is called intrathoracic defibrillation. Placing the electrode pads on the chest wall for defibrillation is called extracorporeal defibrillation. During electrical defibrillation, the position of the electrode pads is crucial. The principle is to ensure that as much myocardial tissue as possible is hit by the electrical current to achieve a better effect.
3. Anterior-lateral defibrillation is usually chosen, where one electrode pad is placed below the right clavicle on the sternum, equivalent to the base of the heart, and the other electrode pad is placed outside the left nipple, equivalent to the apex of the heart. There is only one mode for electrical defibrillation, which is the non-synchronized mode. After electrical defibrillation treatment, the success rate of cardiopulmonary resuscitation will be greatly improved.